Equitable access to prescription medication
No patient should have to decide between filling their prescription or buying food. This principle guides VCH's Medication Affordability Initiative.
Established in 2015, and led by Kimi Manhas, Dr. Lynn Straatman and Dr. Kenneth Gin, the goal of the Medication Affordability Initiative is to create actionable strategies that support patients and care providers address cost-related nonadherence (CRNA).
CRNA is when a patient cannot afford and therefore does not take their prescribed medication. Cost-related nonadherence can include cutting pills, taking lower than prescribed doses, delaying refills and skipping doses. It can also include cutting back on other spending, such as food, bills or rent.
Through collaboration between policymakers, health-care providers, researchers and internal and external stakeholders, the initiative aims to support equitable access to prescription medication using education and engagement strategies.
“We recognized early on that medication affordability is an intricate and multilevel problem," says Kimi Manhas, Clinical Planner at VCH. Kimi spearheaded the project from its conception to its initial funding as a VPSA pilot project.
To tackle CRNA the team had to examine the issue from every level: the patient, the health-care provider and the organization.
At the patient level, they realized that there were people who were not able to afford their prescriptions, who could get sicker and require hospitalization or even die.
“When patients can't afford their medications it leads to increased morbidity and mortality," says Dr. Lynn Straatman, Medical Director, Cardiac Function Clinic, and Interim Medical Coordinator, Vancouver Home Hospice Palliative Care Service at VCH. “This is especially true for patients who are already facing increased healthcare burdens due to other disadvantages in their social determinants of health."
At the provider level, many healthcare providers were unaware of medication affordability issues or solutions; and at the organizational level, many leadership team members were unaware of the impacts of medication affordability, so a systemic approach had not been taken to address the problem.
“We learned that many healthcare providers did not know about the resources available to support patients," says Kimi. “The resources were not easily accessible in one place. If health-care providers have patients who cannot afford their prescription medications, they need a quick and easy way to direct them to the right resources."
Rather than coming up with stop gap solutions, the group has worked to create systemic change so that those most affected by CRNA – women, young adults, Indigenous peoples, those with poorer health statuses and those lacking drug insurance coverage – have more support.
So, what can you do as a physician?
“The first step is to simply ask every patient 'Can you afford your medications?'" says Dr. Straatman. “This simple question lets the patient know that you see them as a whole person. You also need to know what you can do to help: from prescribing medications using the lowest cost possible, to asking about your patient's enrolment in Fair Pharmacare or other programs, to filling out the appropriate special authority forms and determining whether every medication you are prescribing is necessary for their health."
Learn more about the resources and tools created by VPSA's Medication Affordability Initiative. To get involved with the initiative, contact Kimi Manhas (Kimi.Manhas@vch.ca).
Meeting translation needs with an in-house team
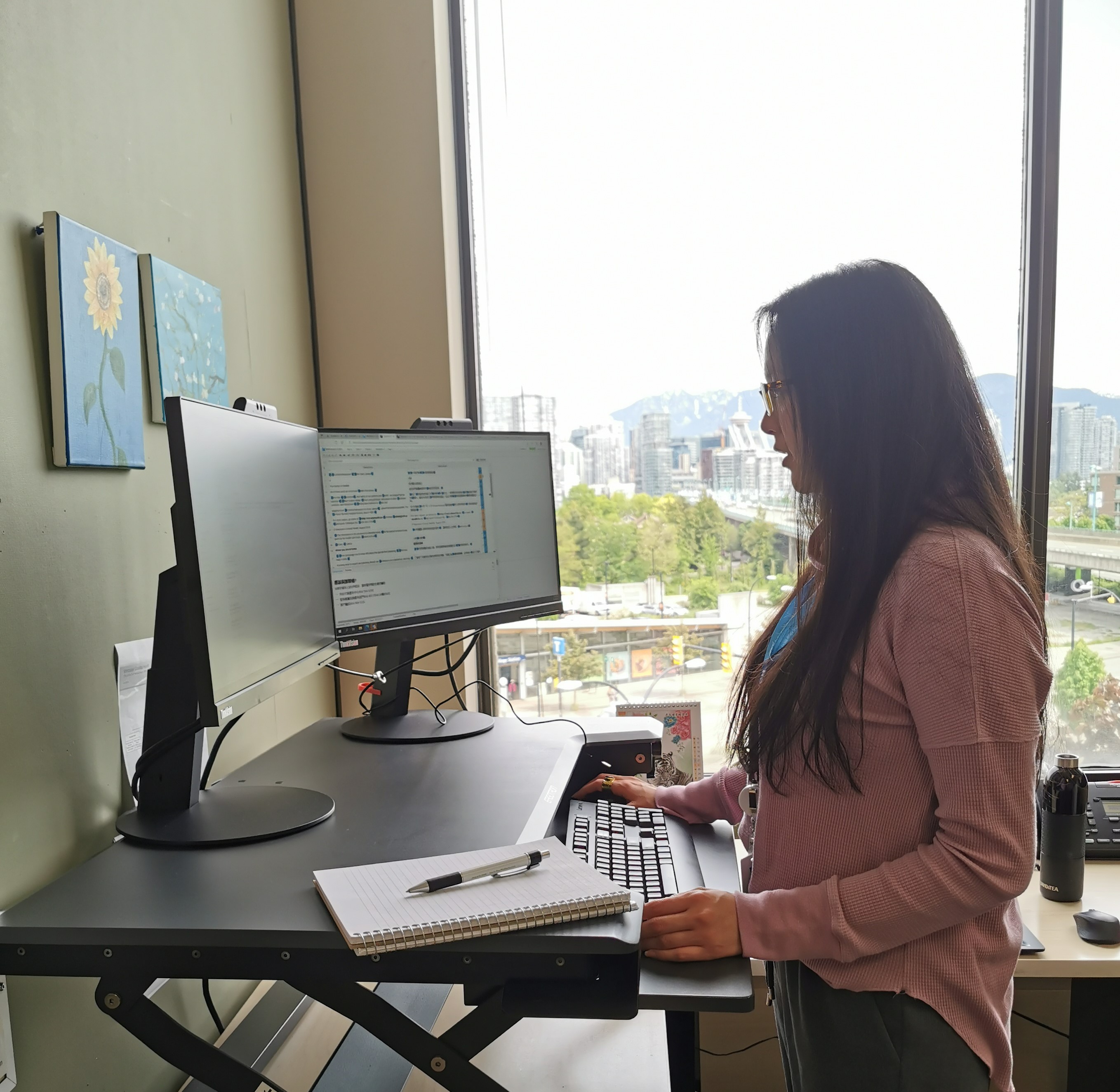
Photo: Rose Jen, Program Leader, Language Services
 Communication is key. Nowhere is that more apparent that in a health-care setting.
Communication is key. Nowhere is that more apparent that in a health-care setting.
Health-care providers need to be able to share detailed information, such as post-operative instructions, and know that their patients understand the information.
In 2020 and 2021, the VCH Community Engagement team worked with stakeholders including, SUCCESS, Immigrant Services Society of BC, the South Vancouver Neighbourhood Health Network, Collingwood Neighbourhood Health Network, and VCH medical staff, on an outreach project to determine what interpreting and translation services would benefit patients.
They heard from stakeholders that to best meet the translation needs of the community, an in-house translation team was needed. Currently, the Language Services Team consists of a program leader, program coordinator and contract translators. The team's goal is to provide a centralized system to ensure translation accuracy and cultural appropriateness across the health authority.
Rose Jen, Program Leader, Language Services, manages the new Language Services Team. As a certified medical interpreter and a medical translator, Rose knows the importance of accuracy in medical translation.
“I have experienced the emotion of relaying difficult information to patients, the importance of accuracy and the real-life consequences of miscommunication," says Rose. “I remember interpreting for a senior patient who needed to use a puffer. It turned out they had almost died because they didn't know how to use it properly. Although an interpreter was present in their first appointment, a translated brochure to refer to when they got home would have made a huge difference in their care."
Having an in-house translation team and using the Translation Style Guide will help ensure consistency. Previously, every clinic did their own translations for materials, which led to inconsistencies in language use, terminologies, register, and tone, amongst other linguistic elements.
Now health-care staff have one place to submit their request and access the Translation Framework to help them determine whether their materials are eligible for translation. By streamlining this intake, it also means that previously translated items can be repurposed across various VCH settings.
“On average, we get about five to six translation requests a month," says Rose. “Keep in mind that each request could have five plus languages (the VCH top five spoken languages are Cantonese and Mandarin (62 per cent), Punjabi (7.2 per cent), Spanish (5.78 per cent) and Vietnamese (5.14 per cent)) that the document needs to be translated into, and some are rather large projects so that adds up."
Since demand is high for translation services, the framework created by Community Engagement, helps health-care providers determine if they need translation services, or if interpreting services would be a better fit for what they need.
Health-care providers should answer yes to the following before requesting translation services from the Language Services Team:
Will the content affect patient/client health care access or outcomes?
Does the content include complex patient care information?
Will the content be relevant for greater than 12 months?
Is the content written using simple language with as little medical jargon as possible?
“Those who request translations might be surprised to learn how long it takes to translate documents," says Rose. “A two-page, double-spaced document takes about a week to complete because we also need to factor in translator availability, proofreading, and editing. The number of words to translate doesn't always reflect the amount of work. Slogans, terms or expressions without context, or documents that are graphic-heavy, typically take longer to complete. Then there needs to be a post-layout proofreading, so typically, the total time for document translation could take around 7-10 business days."
Learn more about how to submit materials for translation to the Language Services Team.
Search and selection process: Using a diversity, equity and inclusion lens
Having an inclusive and representative team of medical staff at VCH is a priority. It is important that medical staff feel a sense of belonging and reflect the populations they serve.
Research shows that culturally safe and appropriate care improves patient health outcomes and the quality of care; it can also enrich provider experiences.
At VCH, having an inclusive and representative team of medical staff is a priority. It is also important to medical leaders that all medical staff feel welcome in their place of work and do not encounter barriers or stigma as they serve our population.
This starts with recruitment and hiring. Though VCH is starting to use a DEI lens in search and selection for medical staff appointments, medical leaders shared barriers and challenges with the VCH Health Authority Medical Advisory Committee (HAMAC) at its meeting in May. Feedback centered on HR supports, adequate skills and training requirements, inclusive job posting language, equitable access to posting platforms and alignment with UBC recruitment processes, when required.
HAMAC is working with Medical Affairs to revise the current standard operating procedure for search and selection to include a stronger focus on DEI, reconciliation and cultural sensitivity. While this is underway, medical leaders and staff are encouraged to contact VCH Medical Affairs or a HAMAC member in your community of care with questions or for support in medical staff search and selection.
Read the May 2022 HAMAC Highlights.
Indigenous birth work is a form of resurgence
Indigenous midwives are working to restore Indigenous birthing practices and contributing to health-related calls to action from Reclaiming Power and Place: The Final Report of the National Inquiry into Missing and Murdered Indigenous Women and Girls.
Not only are Indigenous midwives providing culturally safe care and filling gaps in primary health care services, they are also rebuilding capacity in Indigenous communities to bring birth closer to home and to reclaim the traditional roles of midwives. As part of VCH's Indigenous Health team, midwife members are strategically identifying and fixing gaps in the perinatal health care system. Read the full story on oneVCH.