Dr. Rashmi Chadha, an addiction and pain management specialist at Vancouver Coastal Health (VCH), is passionate about creating a community movement to address the climate emergency.
 In her work, Rashmi has seen firsthand the human impact of the climate crisis.
In her work, Rashmi has seen firsthand the human impact of the climate crisis.
“Many of my patients are people that are homeless," says Rashmi. “Which makes them particularly vulnerable to climate change. This was especially evident last summer when BC experienced extreme heat during the heat dome."
In February 2020, Rashmi co-founded Extinction Rebellion – Health Professionals, which in April 2021, became Doctors for Planetary Health – West Coast. The organization's mission is to remind people of the interconnectedness between human and ecological health.
“I felt that getting a group of health care professionals: physicians, nurse practitioners and medical students together, to do grassroots activism, could be a powerful image," says Rashmi. “As health care professionals, we are seen as a trusted voice within the community, and I thought it would be impactful for the general public to see physicians, in their spare time, protesting for the environment."
Through grassroots activism, the organization hopes to bring attention to the cost that climate crisis inaction is taking on people's health.
On November 4, 2021, the group protested in front of the Legislature in Victoria. Dressed in scrubs, members of Doctors for Planetary Health – West Coast gave their prescriptions for climate action.
They hope to engage change at all levels of the community, from the provincial government, to the health authorities, to other doctors and their patients.
Doctors for Planetary Health – West Coast believe that every decision must be approached with a climate change angle, including decisions made within the health care system.
Rashmi's advice to her fellow medical professionals is to get involved. Join your local Green+ Leaders team and start the conversation for change. Find like-minded colleagues and take your ideas for change to your managers.
“One silver lining of the pandemic," she says, “Is that it has helped people reconnect to nature. When we are not connected to nature, we forget how crucial it is."
More information on Doctors for Planetary Health – West Coast can be found here
Reduction in routine 'group and screens' leads to a greener healthcare system
Photo: Dr. Andrew Shih (Left) and Dr. Jacqueline Trudeau (Right)
Sometimes, the smallest changes can lead to significant outcomes.
 When Drs. Jacqueline Trudeau and Andrew Shih decided to investigate the impact of reducing preoperative group and screens (GRS) for their Physician Led Quality Improvement (PLQI) project, they wanted to help ease the burden placed on patients, but also on the healthcare system as a whole.
When Drs. Jacqueline Trudeau and Andrew Shih decided to investigate the impact of reducing preoperative group and screens (GRS) for their Physician Led Quality Improvement (PLQI) project, they wanted to help ease the burden placed on patients, but also on the healthcare system as a whole.

Andrew, Medical Director and Regional Medical Leader of Transfusion Medicine at Vancouver Coastal Health, explains that their GRS reduction project, to some extent, was born out of the pandemic.
“Most preoperative consultations have been happening virtually due to COVID-19," says Andrew. “However, since the preoperative GRS still needs to be done at the site where the surgery happens, many patients were having to travel long distances, just to get their bloodwork done."
They developed a dashboard tool linking surgical procedures to transfusion rates, to demonstrate that if a patient's bleeding risk was low enough (less than two percent), then the likelihood of requiring a transfusion was also very low, meaning a 'routine' GRS prior wasn't needed prior surgery.
PLQI program advisors Emma Pienaar and Allison Chiu were instrumental in the development of the dashboard tool.
The dashboard was originally born out of a proof-of-concept spreadsheet which Jacqueline herself painstakingly developed, by linking the datasets and applying the concept of minimizing unnecessary GRSs in orthopedic surgeries.
“The goal is to produce a set of shared guidelines based on our local transfusion data," says Andrew. “This will hopefully help surgeons and anesthesiologists decide which patients require a GRS, and which do not."
Not only will patients and physicians be able to save their time and resources, but also, the environmental impact will be greatly reduced as a result.
“There are some key environmental benefits that we are hoping to highlight, from the reduction in carbon emissions resulting from less travel, to the decrease in medical supplies used," says Andrew.
By collaborating with the UBC Planetary Healthcare Lab, they're now expanding the date in the dashboard tool such as the distance a patient travels to obtain their GRS, to determine the environmental impact.
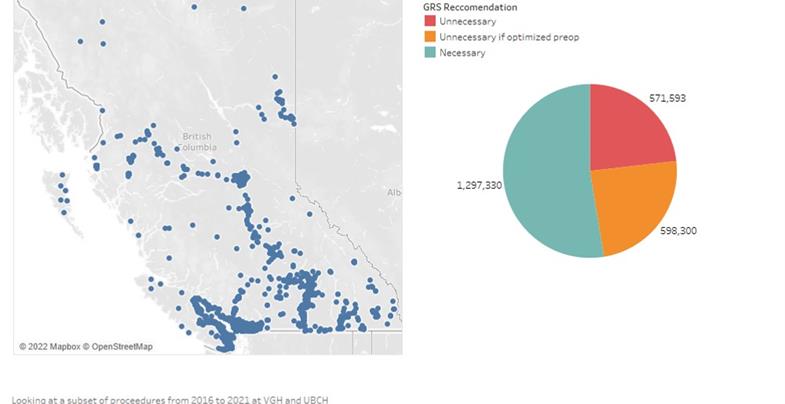
Based on roughly 15 percent of surgeries at UBC Hospital and Vancouver General Hospital (VGH) from 2016 and 2021, the team concluded that patients travelled approximately 571, 593 km for unnecessary GRSs – this equates to an estimated 195.8 tonnes of carbon emissions.
Andrew says the project also highlights inequities within the healthcare system, particularly for those living in smaller, rural and/or remote communities.
“For patients needing to travel to an urban centre for their GRS, this often also means taking one or more days off from work, just to get a blood test done," says Andrew. “So we're hoping to make it possible for these patients to have their initial GRS done where they live, to help lower the burden placed on them."
Traditionally, testing took place at the operating centre to ensure the right patient received the right blood. The team is working with blood banks across the province for testing closer to home. They're developing unique approaches to safely share results for identified peri-operative patients with the operating centres, to help them prepare properly-matched blood.
The team believes collaborating across health authorities will both help reduce the significant time and financial burden for patients in rural areas, and will provide a more welcoming and patient-centered approach.
“Some people living in remote communities, including Indigenous communities, may not feel entirely comfortable accessing care in larger centers, and are often more open to, and accepting of, care provided in their local community," says Andrew.
Andrew and Jacqueline are just two of many health professionals in B.C. and elsewhere working to reduce unnecessary testing for the benefit of patients, the healthcare system, and overall planetary health.
The triple-bottom line: how unnecessary lab testing impacts patients, hospitals and the environment
 Photo: Dr. Karina Spoyalo (Left) and Dr. Janet Simons (Right)
Photo: Dr. Karina Spoyalo (Left) and Dr. Janet Simons (Right)
Have you ever stopped to wonder whether all lab tests ordered for patients are absolutely necessary?
For Dr. Janet Simons, Co-Medical Director, Clinical Informatics, and Internal Medicine Physician at Providence Health Care (PHC), this question has been the focus of much of her work at St. Paul's Hospital (SPH).
“As a medical biochemist, lab medicine is an integral aspect of my work," says Janet. “So I'm constantly questioning, with both hospitalized patients and outpatients, 'do we always need all of the lab tests that are ordered on our patients?'"
She says at SPH, the norm has been to collect blood work from patients every morning, which can be unpleasant for the patient, and is often unimportant for their medical care plan.
“So by inserting a prompt in the system for physicians to choose whether or not to reorder blood work, we reduced the amount of blood we were collecting each day by approximately 30 percent," she says.
Each blood test requires several physical components, including the needle, plastic tubing, sterile coating and paper labels. Due to staffing and supply chain issues caused by the pandemic, some of these are now imported, resulting in additional emissions from shipping.
“You can imagine the environmental impact not only from the amount of waste produced, but also from planes flying across the globe to deliver supplies," says Janet. “Decreasing the amount of blood and other lab tests is a relatively simple, yet highly impactful, means of reducing the carbon footprint of our healthcare system."
The UBC Planetary Healthcare Lab, led by Dr. Andrea MacNeill, creates innovative solutions to tackle the growing environmental effects of the B.C. healthcare system. Dr. Karina Spoyalo, General Surgery Resident at Vancouver General Hospital (VGH) and member of the lab, has been leading a study around eliminating excessive blood work.
“We've been focusing specifically on general surgery inpatients, and we wanted to see how often we've been collecting non-essential blood work," says Karina. “On average, nearly one in five patients in Canada undergo some form of unnecessary blood testing, and this is due to various factors, but ultimately it stems from a lack of standardization."
Their team found that 76 percent of uncomplicated general surgery patients at VGH were receiving unnecessary blood work. They also developed a set of recommendations to guide the appropriate use of lab testing, and avoid unnecessary investigations into patient presentations.
“We calculated the cost of the excess testing to be around $10,000 [over one year], which may not sound like a lot at first, but this is one small subset of patients, in one single division of surgery, at one hospital, in just one year," Karina says.
She says they're also trying to measure the total amount of carbon emissions generated during the lifecycle of each single consumable (a syringe, for example), to accurately determine the environmental impact.
“To me, this is the most interesting aspect, but it's also the most granular. We have to multiply the weight of each consumable by its emission factor, and then consider where it was produced, how it was transported to VGH and where it was discarded/recycled."
Quantifying all the carbon dioxide equivalents produced from each lab test helps demonstrate the positive impact of laboratory stewardship programs on the health of individual patients, and global health communities.
Thanks to curious minds like those of Janet and Karina, we'll be a step closer towards a more environmentally sustainable healthcare system.